 Intracranial Tumors
Intracranial Tumors
Presentation/Diagnosis
- 40 to 60 years of age
- signs and symptoms reflecting increasing ICP (intracranial pressure)
- adult onset seizure disorder
- CT or MRI
Management of Anesthesia
- Prevent undesirable changes in CBF (cerebral blood flow) and ICP.
- Position depends on tumor location
- Supratentorial: supine
- Infratentorial: prone or sitting (BEWARE: greatly increases risk of venous air embolism)
Cerebral Blood Flow
- Normal: 50 ml/100 Gm/min (15% of cardiac output)
- Depends on:
- Cerebral metabolic rate for O2 (CMRO2)
- PaCO2
- Cerebral perfusion pressure
- PaO2
- anesthetic agents
- temperature
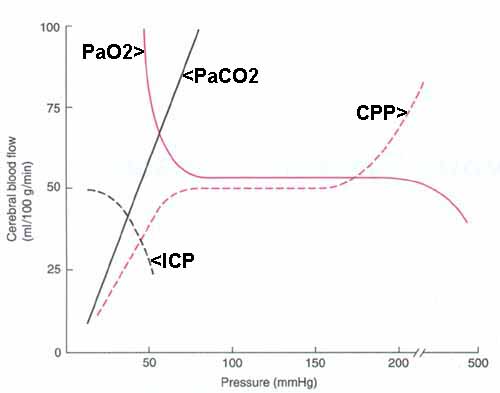
- CBF is proportional to CMRO2
- relationship unaffected by intravenous agents, but
- may be uncoupled by inhalation agents
- PaCO2
- 1 mmHg change in PaCO2 produces 1 ml/100 Gm/min change in CBF (in same direction) but
- transient effect (wanes in 6-8 hours)
- normal patients: for normal CBF maintain normal PaCO2 = 40 mmHg
- CBF and thus ICP may be acutely lowered hyperventilating to lower PaCO2
- Cerebral perfusion pressure (CPP) and autoregulation
- CPP is proportional to mean arterial pressure (MAP)
- if ICP > right atrial pressure (RAP), then
CPP = MAP - ICP - if RAP > ICP, then
CPP = MAP - RAP - normal: autoregulation keeps CBF relatively constant as long as CPP is between 50 and 150 mmHg
- if CPP < 50 mmHg or CPP > 150 mmHg, then CBF is proportional to CPP
- chronic hypertension shifts the CBF-CPP curve to the right so
- higher CPP tolerated but
- lower CPP (< 50 mmHg) may result in too-low CBF
- autoregulatory response
- impaired by intracranial tumors
- not impaired by inhalation anesthetics
- PaO2
- PaO2 < 50 mmHg causes significant increases in CBF
- Anesthetic agents
- inhalation agents
- decrease CMRO2, but
- > 0.6 MAC (minimum alveolar concentration) leads to cerebral vasodilation and dose-dependent increases in CBF
- vasodilation greatest with halothane >> isoflurane, desflurane, sevoflurane
- ketamine
- generally increases CMRO2 and CBF
- if PaCO2 maintained normal in presence of elevated ICP or cerebral trauma, then ketamine does not adversely alter CBF or ICP *
- thiopental
- potent cerebral vasoconstrictor
- decreases CMRO2, CBF, and ICP
- propofol
- decreases CMRO2, CBF, and ICP
- decreased MAP leads to decreases CPP
- etomidate
- decreases CMRO2, CBF, and ICP
- increases EEG activity
- opoids
- depress ventilation, increasing PaCO2 leading to increases in CBF and ICP
- depress level of consciousness
- cause miosis
- inhalation agents
Pressure-volume (elastance) curves
- elastance = (change in pressure)/(change in volume)
- when intracranial compensatory mechanisms are exhauted, small changes in volume lead to dramatic changes in ICP
Intracranial pressure (ICP)
- normal: < 10 mmHg
- to lower elevated ICP, consider:
- elevate head (to encourage venous drainage)
- hyperventilate (effect wanes in 6-8 hours)
PaCO2 25-30 mmHg probably safest ( <20 mmHg: too much vasoconstriction with risk of cerebral ischemia) - drain CSF
- drugs:
- osmotic diuretics
- steroids
- barbiturates
- inhaled anesthetic agents
- dose-dependent increase in CBF and ICP (especially in patients with intracranial tumors)
- hyperventilation to PaCO2 = 30 mitigates to some extent the elevation of ICP caused by inhaled agents
Preoperative evaluation
- Evidence of intracranial hypertension
- nausea and vomiting
- hypertension
- bradycardia
- personality change
- altered level of consciousness
- altered pattern of breathing
- papilledema
- seizures
- MRI or CT
midline shift > 5 mm and/or encroachment on CSF cisterns suggest intracranial hypertension - avoid preop pharmacologic sedation and ventilatory depression
Induction of Anesthesia
- thiopental, propofol, or etomidate -> prompt induction without ICP elevation
- muscle relaxant to facilitate endotracheal intubation and mechanical hyperventilation (BEWARE: coughing causes marked increases in ICP)
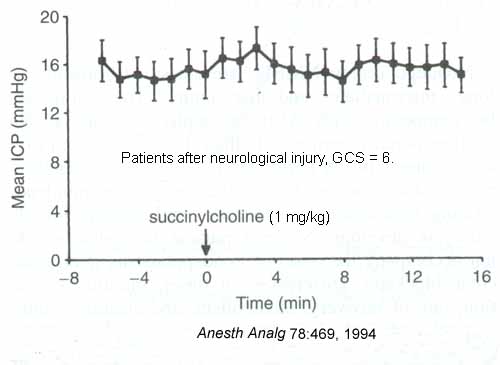
- succinylcholine does not significantly alter CBF or ICP in patients with neurological injury *
- more thiopental, opioids and/or lidocaine 1-2 minutes prior to direct larynogoscopy
- ventilate to PaCO2 25-30
- BEWARE: PEEP may decrease cerebral venous return leading to elevated ICP
Maintenance of anesthesia
- N2O, opioids, benzodiazepines and/or barbiturates
- inhaled agents - isoflurane, desflurane, sevoflurane - at < 0.6 MAC OK with PaCO2 25-30
- in patients with elevated ICP, avoid vasodilators (nitroprusside, nitroglycerine, trimethophan) before the dura is opened
- muscle relaxants (muscle activity may lead to elevated ICP)
- may decide to treat cerebral swelling
- mannitol 0.25-1 Gm/kg IV
- furosemide 0.5-1 mg/kg IV
- thiopental
- head up position
- IV fluids
- minimal, 1-3 ml/kg/hr
- glucose NOT recommended
- may increase cerebral edema
- hyperglycemia worsens cellular ischemic injury
- isotonic crystalloids
- hetastarch OK
Monitors
- standard (including ETCO2) plus:
- arterial line
- maybe ICP monitor
- probably bladder catheter
- sitting position: CVP catheter
Awakening
- avoid coughing, straining
- thiopental or lidocaine
- BEWARE: N2O may cause tension pneumocephalus
- delayed return to consciousness or neurologic deterioration: CT or MRI
Venous Air Embolism (VAE)
- consider whenever head > 5 cm above heart
- transected veins in cut edge of bone or dura may not collapse
- air -> RV -> pulmonary circulation
- decreased pulmonary blood flow, pulmonary edema, bronchoconstriction, cardiovascular collapse, hypoxemia
- paradoxical (air) embolism
- coronary or cerebral circulations
- via patent foramen ovale (PFO) (20-30% of adults have probe-patent foramen ovale)
- detection
- precordial Doppler ultrasound near right upper sternal border is most sensitive non-invasive monitor (detects 0.25 ml)
- trans-esophageal echocardiography is more sensitive, but more invasive and cumbersome
- sudden decrease in ETCO2, incease in ETN2
- gasping, hypotension, dysrhythmias, cyanosis, "mill-wheel" murmur
- treatment
- irrigate operative site with fluid
- apply occlusive material to bone edges
- gently compress internal jugular veins
- head down position
- aspirate air through right atrial catheter (best if tip is at SVC-RA junction)
- discontinue N2O
- inotropes may be needed
- BEWARE: PEEP, by reversing RA-LA pressure gradient, may lead to paradoxical air emboli via PFO